CT Chest (Thorax) - CAM 750
Description
Computed tomography (CT) scans provide greater clarity than regular X-rays and are used to further examine abnormalities found on chest X-rays. They may be used for detection and evaluation of various disease and conditions in the chest, e.g., tumor, inflammatory disease, vascular disease, congenital abnormalities, trauma and symptoms such as hemoptysis.
OVERVIEW
LDCT for Lung Cancer Screening — Screening should be discontinued once a person has not smoked for 15 years or develops a health problem that substantially limits life expectancy or the ability or willingness to have curative lung surgery.
CT and Aneurysm
- Initial evaluation of aneurysm (Erbel, 2014; Hannuksela, 2015; Hiratzka, 2010)
- Echocardiogram shows aneurysm
- Echocardiogram inconclusive of proximal aorta and first-degree relative with thoracic aneurysm
- Chest X-ray shows possible aneurysm
- Follow-up after established thoracic aneurysm (above these sizes surgery is usually recommended) (Erbel, 2014; Hannuksela 2015; Hiratzka, 2010)
- Aortic root or ascending aorta
- 3.5 to 4.5: Annual
- 4.5 to 5.4: Every 6 months
- Genetically mediated (Marfans syndrome, aortic root or ascending aorta)
- 3.5 to 4.0: Annual
- 4.0 to 5.0: Every 6 months
- Descending Aorta
- 4.0 to 5.0 Annual
- 5.0 to 6.0 Every 6 months
- Aortic root or ascending aorta
CT and Interstitial Lung Disease (ACR, 2019) — Radiography of the chest is usually appropriate for the initial imaging of patients who undergo screening and surveillance for lung disease when occupational exposure is present.
Costochondritis (Proulx, 2009) — If physical exam findings are suggestive of costochondritis but the pain is persistent despite conservative care, it should be kept in mind that costochondritis can be recurrent and persistent. It is associated with fibromyalgia. Chest CT should be considered if the findings are not consistent with typical costochondritis, such as fever or elevated inflammatory markers, suggestive of infection or a suspicion of cancer based on history or current findings.
CT for Management of Hemoptysis — High-resolution CT (HRCT) is useful for estimating the severity of hemoptysis, localizing the bleeding site and determining the cause of the bleeding. Its results can be related to the severity of bleeding. The volume of expectorated blood and the amount of blood that may be retained within the lungs without being coughed up are important. HRCT is a way to evaluate the amount of bleeding and its severity. It may also help in the localization of bleeding sites and help in detecting the cause of bleeding.
CT and Solitary Pulmonary Nodules — Solitary pulmonary nodules are abnormalities that are solid, semisolid and non-solid; another term to describe a nodule is focal opacity. CT makes it possible to find smaller nodules and contrast-enhanced CT is used to differentiate benign from malignant pulmonary modules. When a nodule is increasing in size or has spiculated margins or mixed solid and ground-glass attenuation, malignancy should be expected. Patients who have pulmonary nodules and who are immunocompromised may be subject to inflammatory processes.
CT and Empyema — Contrast-enhanced CT used in the evaluation of the chest wall may detect pleural effusion and differentiate a peripheral pulmonary abscess from a thoracic empyema. CT may also detect pleural space infections and help in the diagnosis and staging of thoracic empyema.
CT and Rib Fractures (ACR, 2018) — Chest CT may be useful for characterizing a pathologic fracture, and some features may be helpful in differentiating a primary malignant tumor of bone from metastasis. CT may also be helpful to search for a primary malignancy in patients with a suspected pathologic fracture; however, there is no strong indication that CT serves a significant use as the initial imaging modality to detect pathologic rib fractures.
CT and Occupational Lung Disease (ACR, 2019) — The chest radiograph and CT are complementary in the initial workup of suspected occupational lung disease. When patients with occupational exposures present with respiratory symptoms, chest radiography serves as the primary function of excluding alternative diagnoses, such as infectious pneumonia or pulmonary edema, with HRCT findings offering the best characterization of lung disease.
CT and Tuberculosis — "The chest radiograph is usually the first study performed in patients suspected of having TB. Although frontal and lateral radiographs are often performed in this setting, it has been shown that the lateral radiograph does not improve the detection of findings related to TB. In those with signs or symptoms of disease, the radiographic pattern of upper-lobe or superior-segment lower-lobe fibrocavitary disease in the appropriate clinical setting is sufficient to warrant respiratory isolation and sputum culture for definitive diagnosis. Using radiographs in combination with clinical evaluation results in a high sensitivity for the diagnosis but a relatively low specificity for both latent and active TB. In addition, radiographs may reveal ancillary findings of TB such as pleural effusion or spondylitis. For immunocompromised hosts, particularly those with a low CD4 count, computed tomography (CT) should be considered (ACR, 2016)." CT may be of value in the severely immunocompromised patient with a normal or near-normal radiograph by revealing abnormal lymph nodes or subtle parenchymal disease. Finally, CT may also have a role in identifying patients with latent TB who will be at risk for reactivation disease.
CT and Superior Vena Cava (SVC) Syndrome — SVC is associated with cancer, e.g., lung, breast and mediastinal neoplasms. These malignant diseases cause invasion of the venous intima or an extrinsic mass effect. Adenocarcinoma of the lung is the most common cause of SVC. SVC is a clinical diagnosis with typical symptoms of shortness of breath along with facial and upper extremity edema. Computed tomography (CT), often the most readily available technology, may be used as confirmation and may provide information including possible causes.
CT and Family History of Lung Cancer (Loverdos, 2019) —Family history is equally important. Individuals with a family history of lung cancer among first-degree relatives have been consistently shown to have a two-fold higher risk of developing lung cancer themselves. Those with multiple affected family members diagnosed at younger age appear to be at greater risk.
Policy
This chest CT guideline covers CPT codes 71250 (CT chest without contrast), CT chest with contrast (71260), CT chest without and with contrast (71270) and low-dose CT scan (LDCT) for lung cancer screening (71271). When the case is listed as CT chest in BBI and the clinical scenario or request for LDCT in the office notes meets appropriate use criteria for a LDCT, the LDCT is approvable due to these overlapping CPT codes. Reprocessing of the case to a separate LDCT request is not required.
INDICATIONS FOR CHEST CT
For Annual Lung Cancer Screening
The use of low-dose, non-contrast spiral (helical) multi-detector CT imaging as an annual screening technique for lung cancer is considered medically necessary ONLY when used to screen for lung cancer for certain high-risk asymptomatic individuals when ALL of the following criteria are met:1
- Individual is between 50 – 80 years of age.
- There is at least a 20-pack-per-year history of cigarette smoking.
- If the individual is a former smoker, that individual has quit smoking within the previous 15 years.
Nodule on Initial LDCT2
- If multiple nodules, the largest and type is used for decision
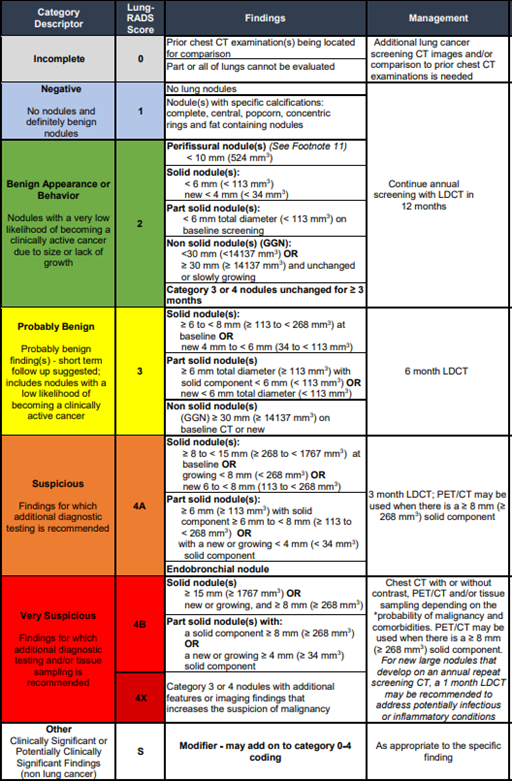
- Follow-up with LDCT as per Lung-RADS® criteria3,4 (Table 1)
Table 1: Lung-RADS Assessment Categories5
Incidental Lung Nodules6
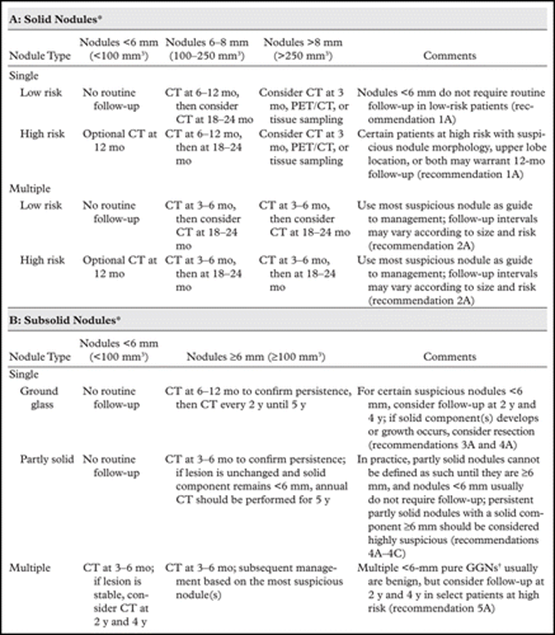
- Incidental pulmonary nodules detected on a nonscreening Chest CT (use Fleischner Table)
- Age ≥ 35 years old — use Fleischner table
- Excludes
- Lung cancer screening (see lung cancer screening guidelines above)
- History of primary cancer (imaging follow-up for surveillance is three months to detect interval nodule growth)
- Immunosuppression (may require a shorter follow-up, such as one month, if suspicion of fulminant infection)
Note: These should not be ordered as low-dose CT
- Incidental pulmonary nodules on non-chest CT
- Nodules > 8 mm or those with very suspicious features need further chest CT as early as possible
- Nodules ≤ 8 mm should follow the Fleischner table
Incidental pulmonary nodules on chest X-ray that are indeterminate (not typical of granulomatous disease) as noted by the radiologist. No time delay between the chest X-ray and the subsequent chest CT needed).
Table 2: 2017 Fleischner Society Guidelines for Management of Incidentally Detected Pulmonary Nodules6
Known Cancer7,8,9
- For follow-up intervals for malignancies10
- Cancer staging (includes unknown primary)
- Cancer restaging
- Suspicious signs or symptoms of recurrence
- Suspected cancer based on prior imaging11
Chest Mass (non-lung parenchymal)12
(Preference should be given to MRI over chest CT for chest wall mass.)
- Mass or lesion, including lymphadenopathy, after non-diagnostic initial imaging
- Thymoma screening in Myasthenia Gravis patients13
Interstitial Lung Disease14,15
- Suspected or known based on restrictive pattern pulmonary function test or signs or symptoms after initial chest X-ray
- Signs or symptoms unresponsive to treatment such as:
- Shortness of breath
- Persistent dyspnea
- Persistent cough
- Monitoring treatment response of known interstitial lung disease
- Patients with known collagen vascular disease16
- Guidance in selection of the most appropriate site for biopsy of diffuse lung disease17
Chronic Cough (> 8 weeks) and chest X-ray completed18
- After evaluation for other causes and failed treatment for those diagnosed with:
- Asthma
- Gastroesophageal reflux disease
- Discontinuation of ACE inhibitors
- Postnasal drip
- Clinical concern for bronchiectasis
Tuberculosis (TB)19
• Known or suspected tuberculosis and initial chest X-ray done
Infection Follow-Up Imaging
- Abscess, empyema or pleural effusions on chest X-ray20
- For evaluation of non-resolving pneumonia or inflammatory disease documented by at least two imaging studies:
- Unimproved with four weeks of antibiotic treatment; OR
- Unresolved at eight weeks21,22
Pneumothorax on Chest X-ray23
Vocal Cord Paralysis on Endoscopic Exam24
- Neck and chest CT is an approvable combo.
Granulomatosis With Polyangiitis (Wegener’s Granulomatosis)25
Vascular Disease
- CT chest is not preferred study for vascular disease, CTA should be considered. See chest CTA guideline.
- Chest CT can be used to detect and follow up thoracic aortic aneurysms. See Background section.
Suspected Pulmonary Embolism (PE)26
- Chest CT not approvable for PE
Congenital Malformations
- Thoracic malformation on chest X-ray27
- Congenital Heart Disease with pulmonary hypertension28
Hemoptysis After X-ray Completed29,30
Pre-operative/Procedural Evaluation
- Pre-operative evaluation for a planned surgery or procedure
- Pre-operative evaluation for electromagnetic navigation bronchoscopy31
Post-Operative/Procedural Evaluation
- Post-surgical follow-up when records document medical reason requiring additional imaging
Chest Wall Pain (after initial evaluation with chest X-ray and/or rib films)32
- History of known or suspected cancer
- Signs and symptoms of infection, such as:
- Accompanying fever
- Elevated inflammatory markers
- Known infection at other sites
Chest CT and COVID-19 (Coronavirus)
- Acute COVID-19
- Imaging is not indicated in patients suspected of having coronavirus disease (COVID-19) and mild clinical features unless they are at risk for disease progression.
- Imaging is indicated in a patient with COVID-19 and worsening respiratory status.
- In a resource-constrained environment, imaging is indicated for medical triage of patients suspected of having COVID-19 who present with moderate-to-severe clinical features and a high pretest probability of disease.
- Long (Chronic) COVID-19 (See Overview.)
- Prior history of COVID-19 with hypoxia or impaired lung function of follow-up33
- Restricted diffusion on pulmonary function test (would need a HRCT, or High Resolution CT)
- Low oxygen saturation and a chest X-ray was done
- Known fibrosis with continued symptoms
- Prior history of COVID-19 with hypoxia or impaired lung function of follow-up33
Combination of Studies With Chest CT
- Abdomen CT/Pelvis CT/Chest CT/Neck MRI/Neck CT With MUGA — Known tumor/cancer for initial staging or evaluation before starting chemotherapy or radiation treatment
- Neck and Chest CT — Neck and chest CT is an approvable combo with vocal cord paralysis and concern for recurrent laryngeal nerve lesion
References
- American College of Chest Physicians (ACCP). Chest the 83rd annual meeting of the American College of Chest Physicians, Toronto, Ontario. 2017.
- American College of Radiology (ACR). ACR Appropriateness Criteria®. https://acsearch.acr.org/list. Published 2014.
- American College of Radiology (ACR). ACR Appropriateness Criteria®. https://acsearch.acr.org/list. Published 2018.
- American College of Radiology (ACR). ACR Appropriateness Criteria®. Acute Chest Pain—doi: https://doi.org/10.1016/j.jacr.2017.02.027.
- American College of Radiology (ACR). ACR Appropriateness Criteria®. Hemoptysis. Revised 2019. https://acsearch.acr.org/docs/69449/Narrative/.
- American College of Radiology (ACR). ACR Appropriateness Criteria®. Imaging of Possible Tuberculosis. 2016. https://acsearch.acr.org/docs/3099187/Narrative/.
- American College of Radiology (ACR). Lung - RADS Assessment Categories v1.1. 2019. https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/Lung-Rads.
- American College of Radiology (ACR). ACR Appropriateness Criteria®. Occupational Lung Diseases. Revised 2019. https://acsearch.acr.org/docs/3091680/Narrative/.
- American College of Radiology (ACR). ACR-STR Practice Parameter for the Performance of High-Resolution Computed Tomography (HRCT) of the Lungs in Adults, Resolution 17. Revised 2015.
- Antoniou KM, Margaritopoulos G, Economidou F, et al. Pivotal clinical dilemmas in collagen vascular diseases associated with interstitial lung involvement. Eur Resp J. 2009; 33:882-96.
- Barman M. Acute aortic dissection. Eur Soc Cardiol. 2014 July 2; 12(25).
- Bryl B, Barlow E, Davies H. P182 Follow up chest X-rays (CXR) after community acquired pneumonia (CAP): Are they done and are they useful? BMJ. 2018; 73(4).
- Bueno J, Landeras L, Chung JH. Updated Fleischner Society guidelines for managing incidental pulmonary nodules: Common questions and challenging scenarios. Radiographics. 2018;38(5):1337-1350. doi:10.1148/rg.2018180017.
- Carter BW, Lichtenberger JP, Benveniste MK, et al. Revisions to the TNM staging of lung cancer: Rationale, significance, and clinical application. RadioGraphics. 2018; 38:374–391. 13— Chest Ceriani E, Combescure C, Le Gal G, et al. Clinical prediction rules for pulmonary embolism: a systematic review and meta-analysis. J Thromb Hemost. 2010; 8(5):957-970. doi: 10.1111/j.1538-7836.2010.03801.x.
- Corrigan D, Prucnal C, Kabrhel C. Pulmonary embolism: The diagnosis, risk-stratification, treatment and disposition of emergency department patients. Clin Exp Emerg Med. 2016 Sep; 3(3):117–125.
- Cohen R, Mena D, Carbajal-Mendoza R, et al. Superior vena CVA syndrome: A medical emergency? Int J Angiol. 2008; 17(1):43-46. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2728369/pdf/ija17043.pdf.
- De Koning HJ, Meza R, Plevritis SK, et al. Benefits and harms of computed tomography lung cancer screening strategies: A comparative modeling study for the U.S. Preventative Services Task Force. Ann Int Med. March 4, 2014; 160(5):311-320. doi: 10.7326/M13-2316.
- Dean NC, Griffith PP, Sorensen JS, et al. Pleural effusions at first ED encounter predict worse clinical outcomes in patients with pneumonia. Chest. 2016; 149(6):1509.
- Dogan DO, Berk S, Gumus C, et al. A longitudinal study on lung disease in dental technicians: What has changed after seven years? Int J Occup Med Environ Health. 2013; 26:693-701.
- Dyer DS, Khan AR, Mohammed TL. ACR Appropriateness Criteria on chronic dyspnea: Suspected pulmonary origin. J Thorac Imaging. 2010 May; 25(2):W21-3.
- Erbel R, Aboyans V, Boileau C, et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur Heart J. 2014; 35(41):2873. Epub 2014 Aug 29.
- Ferreira TdA, Chagas ISS, Ramos RTT, et al. Congenital thoracic malformations in pediatric patients: Two decades of experience. J Bras Pneumol. 2015 Mar-Apr; 41(2):196-199.
- Friedman T, Quencer KB, Kishore SA, et al. Malignant venous obstruction: Superior vena cava syndrome and beyond. Semin Intervent Radiol. 2017; 34(4):398. Epub 2017 Dec 14.
- Greco FA, Oien K, Erlander M, et al. Cancer of unknown primary: Progress in the search for improved and rapid diagnosis leading toward upper patient outcomes. Ann Oncol. 2012; 23:298-304.
- Hannuksela M, Stattin EL, Johansson B, et al. Screening for familial thoracic aortic aneurysms with aortic imaging does not detect all potential carriers of the disease. Aorta (Stamford). 2015 Feb; 3(1):1–8. 1
- Hiratzka LF, Bakris GL, Beckman JA , et al. 2010 ACCF / AHA / AATS / ACR / ASA / SCA / SCAI / SIR / STS / SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. Circulation. 2010; 121(13):e266.
- Hong SJ, Kim TJ, Nam KB, et al. New TNM staging system for esophageal cancer: What chest radiologists need to know. RadioGraphics. 2014; 34(6).
- Kalemkerian GP, Akerley W, Bogner P, et al. Small Cell Lung Cancer - NCCN Clinical Practice Guidelines in Oncology. February 2013; 1-48. http://www.nccn.org/professionals/physician_gls/pdf/sclc.pdf.
- Ketai LH, Mohammed TL, Kirsch J, et al. ACR Appropriateness Criteria® Hemoptysis. J Thorac Imaging. 2014 May; 29(3):W19-22.
- Khan KA, Nardelli P, Jaeger A, et al. Navigational bronchoscopy for early lung cancer: A road to therapy. Adv Ther. 2016; 33:580-596.
- Ko Y, Lee HY, Park YB, et al. Correlation of microbiological yield with radiographic activity on chest computed tomography in cases of suspected pulmonary tuberculosis. PloS One. 2018 Aug 9; 13(8):e0201748.
- Konstantinides SV, Torbicki A, Agnelli G, et al. 2014 ESC Guidelines on the diagnosis and management of acute pulmonary embolism: The Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). Eur Heart J. 2014 Nov 14; 35(43):3033–80.
- Kovalchik SA, Tammemagi M, Berg CD, et al. Targeting of low-dose CT screening according to the risk of lung-cancer death. NEJM. July 2013; 369(3):245-54. doi: 10.1056/NEJMoa1301851.
- Kumar R. Myasthenia gravis and thymic neoplasms: A brief review. World J Clin Cases. 2015 Dec 16; 3(12):980–83.
- Latief KH, White CS, Protopapas Z, et al. Search for a primary lung neoplasm in patients with brain metastasis: Is the chest radiograph sufficient? AJR Am J Roentgenol. 1997; 168:1339–44.
- Lee SC, Jain PA, Jethwa SC, et al. Radiologist’s role in breast cancer staging: Providing key information for clinicians. RadioGraphics. 2014; 34(2).
- Li J, Li C, Li J. Thoracic manifestation of Wegener's granulomatosis: Computed tomography findings and analysis of misdiagnosis. Exp Ther Med. 2018 Jul; 16(1):413–419.
- Little BP, Gilman MD, Humphrey KL, et al. Outcome of recommendations for radiographic follow-up of pneumonia on outpatient chest radiography. AJR. 2014; 202:54–59.
- Loverdos K, Fotiadis A, Kontogianni C, et al. Lung nodules: A comprehensive review on current approach and management. Ann Thorac Med. 2019 Oct-Dec; 14(4):226-238.
- MacMahon H, Naidich DP, Goo JM, et al. Guidelines for management of incidental pulmonary nodules detected on CT images: From the Fleischner Society 2017. Radiology. 2017 July; 284(1):228-243. Epub 2017 Feb 23. doi: 10.1148/radiol.2017161659.
- Mazzone PJ, Silvestri GA, Patel S, et al. Screening for lung cancer CHEST guideline and expert panel report. CHEST. 2018; 153(4):954-985.
- Melamed KH, Fereidoun AF, Barjakterevic I, et al. Diagnostic value of quantitative chest CT in a case of spontaneous pneumothorax. Chest. 2017; 152(5):e109-114.
- Miller A, Warshaw R, Nezamis J. Diffusing capacity and forced vital capacity in 5,003 asbestos-exposed workers: Relationships to interstitial fibrosis (ILO profusion score) and pleural thickening. Am J Ind Med. 2013; 56:1383-93.
- Mullan CP, Madan R, Trotman-Dickenson B, et al. Radiology of chest wall masses. AJR. 2011; 197(3).
- National Comprehensive Cancer Network (NCCN). NCCN Imaging Guidelines. 2019. https://www.nccn.org/store/login/login.aspx?ReturnURL=/professionals/imaging/content.
- Nishino M, Itoh H, Hatabu H. A practical approach to high-resolution CT of diffuse lung disease. Eur J Radiol. 2014; 83(1):6-19.
- Paquette CM, Manos DC, Psooy BJ. Unilateral vocal cord paralysis: A review of CT findings, mediastinal causes, and the course of the recurrent laryngeal nerves. RadioGraphics. 2012; 32(3).
- Pascall E, Tulloh RMR. Pulmonary hypertension in congenital heart disease. Future Cardiol. 2018 Jul; 14(4):343–353.
- Pratter MR, Abouzgheib W, Akers S, et al. An algorithmic approach to chronic dyspnea. Respir Med. 2011; 105:1014-21.
- Proulx AM, Zryd TW. Costochondritis: Diagnosis and treatment. Am Fam Physician. 2009;80(6):617-620.
- Pynnonen MA, Gillespie MB, Roman B, et al. Clinical practice guideline: Evaluation of the neck mass in adults. Otolaryngol Head Neck Surg. 2017; 157(2 Suppl):S1.
- Rubin GD, Ryerson CJ, Haramati LB, et al. The Role of Chest Imaging in Patient Management during the COVID-19 Pandemic: A Multinational Consensus Statement from the Fleischner Society. Radiology 2020 July; 296(1):172-180.
- Singh B, Mommer SK, Erwin PJ, et al. Pulmonary embolism rule-out criteria (PERC) in pulmonary embolism--revisited: A systematic review and meta-analysis. Emerg Med J. 2013 Sep; 30(9):701-6. doi: 10.1136/emermed-2012-201730. Epub 2012 Oct 4.
- Tsao YC, Liu SH, Tzeng IS, et al. Do sanitary ceramic workers have a worse presentation of chest radiographs or pulmonary function tests than other ceramic workers? J Formos Med Assoc. 2017; 116:139-44.
- Turner RD, Bothamley GH. Chronic cough and a normal chest X-ray - a simple systematic approach to exclude common causes before referral to secondary care: a retrospective cohort study. NPJ Prim Care Respir Med. 2016; 26:15081.
- U.S. Preventive Services Task Force (USPSTF). Lung Cancer: Screening. Final recommendation statement, March 9, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening.
- Vij R, Strek ME. Diagnosis and treatment of connective tissue disease-associated interstitial lung disease. Chest. 2013; 143(3):814.
- Winzenberg T, Jones G, Callisaya M. Musculoskeletal chest wall pain. Aust Fam Physician. 2015 Aug; 44(8):540-4.
- Wood DE, Eapen GA, Ettinger DS, et al. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines™). National Comprehensive Cancer Network. 2012; 10:240-265. http://www.jnccn.org/content/10/2/240.full.pdf+html.
- Yang C, Liu R, Ming X, et al. Thoracic organ doses and cancer risk from low pitch helical 4- dimensional computed tomography scans. Biomed Res Int. 2018 Sep 24; 2018:8927290. doi: 10.1155/2018/8927290. eCollection 2018.
- Yankelevitz DF, Smith JP. Understanding the core result of the National Lung Screening Trial. NEJM. May 2013; 368(18):1757. doi: 10.1056/NEJMc1213744.
- Yoo S, Lee MH, White C. MDCT evaluation of acute aortic syndrome. Radiol Clin North Am. 2010; 48(1):67-83. doi: 10.1016/j.rcl.2009.09.006.
Coding Section
| Code | Number | Description |
| CPT | 71250 | Computed tomography, thorax; without contrast material |
| 71260 | Computed tomography, thorax; with contrast material(s) | |
| 71270 | Computed tomography, thorax; without contrast material, followed by contrast material(s) and further sections | |
| 71271 (effective 01/01/2021) | Computed tomography, thorax; low dose for lung cancer screening; without contrast material(s) | |
| G0297 | Low dose ct scan (ldct) for lung cancer screening |
Procedure and diagnosis codes on Medical Policy documents are included only as a general reference tool for each policy. They may not be all-inclusive.
This medical policy was developed through consideration of peer-reviewed medical literature generally recognized by the relevant medical community, U.S. FDA approval status, nationally accepted standards of medical practice and accepted standards of medical practice in this community, Blue Cross Blue Shield Association technology assessment program (TEC) and other non-affiliated technology evaluation centers, reference to federal regulations, other plan medical policies, and accredited national guidelines.
"Current Procedural Terminology © American Medical Association. All Rights Reserved"
History From 2019 Forward
| 12/16/2022 | Annual review, addition of single ventricle heart disease coverage criteria, No other changes. |
|
12/15/2021 |
Annual review updating existing information regarding Fleischner criteria and Lung Rads. Also adding section related to COVID 19. Updating description and references. |
|
12/10/2020 |
Updated coding with 2021 codes. No other changes. |
|
12/01/2020 |
Annual review, policy updated for clarity and also adding verbiage regarding low dose CT scanning previously in CAM 60130. Entire policy updated to encompass that addition. |
|
12/03/2019 |
New Policy |